INTRODUCTION
The possibility that one might have an illness bring it own anxieties especial where the person has enjoyed good health previously .If the illness has long term implication then a number of anxieties will surface incase of HIV infection these might include shock
On hearing the diagnosis and considering its implication
Through disappointment on not hearing good news
Anxiety fear due to.
Not knowing what course the infection will take
Worrying about the effects of the treatment /medication
Rejection by family /friends community
Isolation through sexual rejection because of the tears of others concerning infection
Anticipating the partner /family inability to cope with the situation
Concerns about job and or skill losses
Despairs because of
Little hope of cure
Persistent worries about ones inevitable physical decline
Recriminations about being infected and /or spreading the infecting
The limiting effects of the virus
The effect on ones family of being infected
The stigma of being HIV infected
Areas Of counseling.
The two main areas of HIV counseling are;
Educating the infected person so that they will understand the nature of their problems explanation of the available treatment options; outlining ways to prevent others from being infected by them and
Support through anxieties and other physical need meets by people in the cause of their illness.
Counseling opportunities will exist at different stage and provided by different individuals.
Appropriate counseling intervention include
Initial attendance at a clinic or medical centre where the at risk person will have the HIV testing procedures explained.
Personal counseling of the HIV-positive person and the partner family where this is possible and applicable
Available treatment regimes
Instruction is safer sexual practices
Explanation of the development and effect of opportunistic infection and their delay /treatment
Counseling the family of bereaved
Support Networks
Counselors and counseling facilities vary from country to country so there is hardly a standard approach
All community agencies should be alert to their opportunities to provide support to the sick in their midst and to help people with HIV/Aids and their dependants.
This network of support will include:
Families, friends work colleagues
Medical and paramedical staff
Social service charitable organizations
Professional counselor/psychologists
Faith communities
Special organization working specifically with HIV Aids infected people and their families.
Counseling material and messages will need to be particularly relevant to specific target groups whether these be families, women sex workers or youth
Prevention and control of HIV /AIDs
HIV prevention services seem to work best when all the stakeholders are involved in implementation of the strategies .In. Kenya the Interpersonal donor partners local and international NGO’s faith –best organization are involved in activities and service to prevent HIV/Aids
Some of the activities implemented by this organization include:
- Basic evaluation and dissemination of information about HIV.
- Communication about behavior change.
- Community mobilization to change social norms
- Training youths and adolescent in life skill and behavior change e.g. being assertions responsibility accountability social skill ways of relating to others developing a positive mage.
- Peer education and youth to youth initiatives
- Voluntary counseling and testing (V.C.T)
- Prevention and treatment of other sexually transmitted diseases.
- Prevention of mother to child transmission
- Prevention of transfusion in medical settings including are blood transfusion and proper injection control
- Condom education and distribution promotion.
Prevention and control strategies used in Kenya.
- V.C.T as a prevention strategy it is a powerful weapon in the fight against HIV/AIDs since it is associated with behavior change that reduces HIV transmission and serves as a point of entry into care for those testing positive through the joint effort of stakeholders
There has been rapid increase of V.C.T sites in Kenya in the year 2008
V.C.T services are offered through site registration by the ministry of health as an effort to increase the number of people who are tested and to expand access to Aids case and treatment.
The National V.C.T programme use for models of services delivery.
Intergrated -Intergarded site are V.C.T centre which are located within the ground of health facilities such as hospital health centers or dispensaries .There are main advantages include.
Easier referral to medical care service
Low start up cost that allows for an increasing number of people being tested and accessing AIDs core and treatment.
Short coming of integrated sites includes
Health workers
They may have more urgent medical problems to attend to and cannot develop enough time to VCT
Stand alone site –This sites are not usually with existing medical Institution usually have staff denoted to V.C.T, They largely operated by NGOs agencies and they usually located at intensely populated urban areas.
Advantages
They staff can work full time on VCT service
They have donor funds that facilitate their community approach site.
Are V.C.T centers either intergraded into other social service or implanted as a souls activity of a local community based organization (CBOS)
Mobile sites
V.C.T services are provided as an outreach to remote to reach communities.
Benefits of V.C.T
Helps in prevention of transmission of HIV serves as a flat form for care and treatment of Aids
Helps in planning for individual organization as well as the government
Help in identifying the number of HIV infected persons and ways of addressing or promoting prevention of transmission
It is enhancing referral of HIV position client for proper care and T.B prevention.
Prevention of transmission through blood
Blood transfusion often is a life saving intervention but it comes with a risk because it can transmit Infection if safety mercies are not followed
Safety measures include
Blood screening
Sterilization of needle and syringes before using and discarding after each subsequent use
Prevention of mother to child transmission (PMTC)
Mother to child transmission of his is responsible for most HIV infection in children a pregnant. Women who is HIV infected is 30-45% likely to transmit HIV to her newbornchild. The baby can be infected during pregnancy labor and delivery or through breast milk.
Intervention to reduce transmission of HIV include
Prevent HIV infection in women.
The best way to prevent mother to child is to prevent the women from being affected this include engaging in sex.
For women to have a single and uninfected sexual partners
For young women pregnant women and lactating women to use condoms consistently and properly
Reduce the number of HIV exposed pregnancy women who are HIV infected can use family planning methods to prevent pregnancy
QUESTION
Define HIV counseling?
Discuss the procedure of HIV counseling?
What are the roles of client in the session?
HIV & AIDS Vulnerable Groups
AIDS is caused by HIV, a virus that can be passed from person to person through sexual fluids, blood and breast milk.
Worldwide, the majority of HIV infections are transmitted through sex between men and women, and half of all adults living with HIV are women. Certain groups of people have been particularly affected and these include people who inject drugs, sex workers and men who have sex with men.
HIV particularly affects adolescents and young people, who accounted for 39 percent of all new infections and 15 percent of all people living with HIV in 2012. 1 AIDS-related deaths among young adults have an especially damaging impact on their families and communities: skills are lost, workforces shrink and children are orphaned.
In some countries in sub-Saharan Africa, life expectancies have fallen below 40 years, whereas they would have been above 60 without the epidemic. Roughly 17.8 million children have lost at least one parent to AIDS-related illnesses. 2
Apart from inadequate funding, other major obstacles to reducing the vulnerability of these populations to HIV include weak infrastructure and shortages of healthcare workers in the worst affected countries. Political or cultural attitudes are also significant. For example, some authorities are opposed to condom promotion, while others refuse to support needle exchanges for people who inject drugs. Many are also reluctant to provide young people with adequate education about sex and sexual health.
Stigma and discrimination particularly affects these vulnerable groups. People known to be living with HIV are often shunned or abused by community members, employers even healthcare workers. As well as causing much personal suffering, this sort of prejudice discourages people from seeking HIV testing, treatment and care, undermining efforts to tackle the epidemic.
AIDS Stake holders- Institutions Involved in HIV/AIDS Reponses
At the national level, the state policy in the area of HIV/AIDS is implemented through the National Programme on Prevention and Control of HIV/AIDS and STI, which determines national strategies of priority for prevention, epidemiological surveillance and treatment. The structure of the institutional framework of the NAP is rather complex. The main executors of the state policy in the area of HIV/AIDS and STI are the Government, local public administration authorities, Ministry of Health and Social Protection and other Ministries, NGOs, mass media, etc. An important contribution is carried out by international organizations, such as UNAIDS and most UN agencies, GFATM/WB, Soros Foundation Moldova, SIDA, etc.
National AIDS Stakeholders and their Role
National Coordination Council and NCC Secretariat
Development, integration, correlation and monitoring of activities under the NAP
Government and its Ministries
- Capacity building related to national response to HIV/AIDS/STI;
- Support to the consolidation of NGO networks which are working in the field of HIV/AIDS/STI and people living with HIV/AIDS;
- Priority financing, political support of HIV/AIDS activities;
- Focal points and HIV related responsibilities under several ministries;
- M&E
Local Public Administration Authorities
- Regional interdepartmental, multisectoral HIV/AIDS/STIs committees;
- Earmarking in local budgets for HIV/AIDS activities;
- Contribution to regional programmes in the field.
Mass Media
- Promote and make use of non-discriminatory language in HIV/AIDS/STIs
- Communication activities.
National Centre for Public Health
- Evaluation of population health, prognosis as to the evolution of basic indicators and sanitary-epidemiological statistics;
- Elaboration of prevention programmes at national and territorial levels;
- Fighting negative effect of harmful environment and production factors;
- Cooperation with other medical-sanitary national and international institutions of common and global interest;
- Exchange of experience and information.
Public Institution “UCIMP”
- Strengthening of the public health through reforming the health system;
- Development of the institutional capacities;
- Fighting negative effect of harmful environment and production factors;
- Support to the National Programmes on Prevention and Control of HIV/AIDS/STI and TB and National Programmeon Blood Transfusion Safety.
Rayon Centres for Preventive Medicine
- Epidemiological surveillance in territories;
- Elaboration and implementation of preventive measures;
- Organization and coordination activities with other medical institutions.
National AIDS Centre
- Analysis of the epidemiological situation, maintenance of official statistics;
- Elaboration of methods in all the areas of activity;
- Confirmation and reference tests for HIV/AIDS;
- Training and seminars on HIV/AIDS for family doctors.
Republican Dermato-Venerological Dispensary
- ARV treatment;
- Treatment of opportunistic infections.
National Centre for Health Management
- Health system strengthening;
- Scientific research coordination in the field of public health;
- Development of the legislative framework in public health.
Monitoring and Evaluation Unit on HIV/AIDS
- Development of M&E plans for the National AIDS Programmes, UNGASS reports, etc.
NGOs
- Grassroots activities;
- Wide range of prevention, care, support and rehabilitation projects in HIV/AIDS related areas;
- Lobby and advocacy.
International organizations
- Financial and technical assistance.
Association “Positive initiative”
“Positive initiative” is a new created association that represents a network within the organizations with a reach experience in the field of HIV, especially working and providing services for MARPS (Most at Risk populations), people living with HIV, IDU, women and children HIV+ or affected by HIV.
Association “Youth for Right to Life”, Balti
Association “Youth for Right to Life”, Balti is an NGO from Balti, Republic of Moldova, that more than one decade works in the field of HIV prevention, drug abuse and social assistance
HIV Strains: Types, Groups and Subtypes
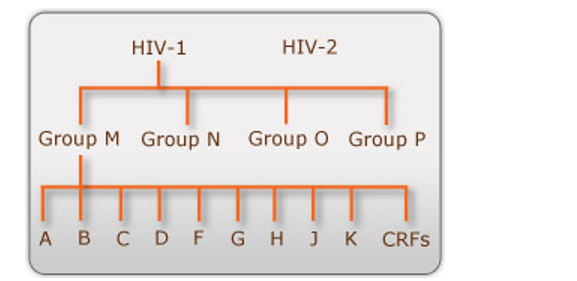
HIV types, groups and subtypes
HIV is a highly variable virus which mutates very readily. This means there are many different strains of HIV, even within the body of a single infected person.
Based on genetic similarities, the numerous virus strains may be classified into types, groups and subtypes.
What is the difference between HIV-1 and HIV-2?
There are two types of HIV: HIV-1 and HIV-2. Both types are transmitted by sexual contact, through blood, and from mother to child, and they appear to cause clinically indistinguishable AIDS. However, it seems that HIV-2 is less easily transmitted, and the period between initial infection and illness is longer in the case of HIV-2.
Worldwide, the predominant virus is HIV-1, and generally when people refer to HIV without specifying the type of virus they will be referring to HIV-1. The relatively uncommon HIV-2 type is concentrated in West Africa and is rarely found elsewhere.
How many subtypes of HIV-1 are there?
The strains of HIV-1 can be classified into four groups: the “major” group M, the “outlier” group O and two new groups, N and P. These four groups may represent four separate introductions of simian immunodeficiency virus into humans.
HIV types, groups and subtypes
Group O appears to be restricted to west-central Africa and group N – a strain discovered in 1998 in Cameroon – is extremely rare. In 2009 a new strain closely relating to gorilla simian immunodeficiency virus was discovered in a Cameroonian woman. It was designated HIV-1 group P. More than 90 percent of HIV-1 infections belong to HIV-1 group M and, unless specified, the rest of this page will relate to HIV-1 group M only.
Within group M there are known to be at least nine genetically distinct subtypes (or clades) of HIV-1. These are subtypes A, B, C, D, F, G, H, J and K.
Occasionally, two viruses of different subtypes can meet in the cell of an infected person and mix together their genetic material to create a new hybrid virus (a process similar to sexual reproduction, and sometimes called “viral sex”). Many of these new strains do not survive for long, but those that infect more than one person are known as “circulating recombinant forms” or CRFs. For example, the CRF A/B is a mixture of subtypes A and B.
The classification of HIV strains into subtypes and CRFs is a complex issue and the definitions are subject to change as new discoveries are made. Some scientists talk about subtypes A1, A2, A3, F1 and F2 instead of A and F, though others regard the former as sub-subtypes.
What about subtypes E and I?
One of the CRFs is called A/E because it is thought to have resulted from hybridization between subtype A and some other “parent” subtype E. However, no one has ever found a pure form of subtype E. Confusingly, many people still refer to the CRF A/E as “subtype E” (in fact it is most correctly called CRF01_AE).
A virus isolated in Cyprus was originally placed in a new subtype I, before being reclassified as a recombinant form A/G/I. It is now thought that this virus represents an even more complex CRF comprised of subtypes A, G, H, K and unclassified regions. The designation “I” is no longer used.
Where are the different subtypes and CRFs found?
The HIV-1 subtypes and CRFs are typically associated with certain geographical regions, with the most widespread being subtypes A and C. As studies have shown, individuals are increasingly presenting with sub-types not native to the country of diagnosis. For example, a rise of non-B sub-types among men who have sex with men (MSM) in the UK has been identified.
- Subtype A and CRF A/G predominate in West and Central Africa, with subtype A possibly also causing much of the Russian epidemic.
- Historically, subtype B has been the most common subtype/CRF in Europe, the Americas, Japan and Australia and is the predominant sub-type found among MSM infected in Europe. Although this remains the case, other subtypes are becoming more frequent and now account for at least 25 percent of new HIV infections in Europe.
- Subtype C is predominant in Southern and East Africa, India and Nepal. It has caused the world’s worst HIV epidemics and is responsible for around half of all infections.
- Subtype D is generally limited to East and Central Africa. CRF A/E is prevalent in South-East Asia, but originated in Central Africa. Subtype F has been found in Central Africa, South America and Eastern Europe. Subtype G and CRF A/G have been observed in West and East Africa and Central Europe.
- Subtype H has only been found in Central Africa; J only in Central America; and K only in the Democratic Republic of Congo and Cameroon.
As a Belgium study highlighted, local epidemics can be better understood if sub-types, patient demographics and transmission routes are recorded. Furthermore, the availability of this data can be used to target risk groups more accurately and to improve the effectiveness of prevention strategies.
Are more subtypes likely to “appear”?
It is almost certain that new HIV genetic subtypes and CRFs will be discovered in the future, and indeed that new ones will develop as virus recombination and mutation continue to occur. The current subtypes and CRFs will also continue to spread to new areas as the global epidemic continues.
The implications of variability
Does subtype affect disease progression?
A study presented in 2006 found that Ugandans infected with subtype D or recombinant strains incorporating subtype D developed AIDS sooner than those infected with subtype A, and also died sooner, if they did not receive antiretroviral treatment. The study’s authors suggested that subtype D is more virulent because it is more effective at binding to immune cells.This result was supported by another study presented in 2007, which found that Kenyan women infected with subtype D had more than twice the risk of death over six years compared with those infected with subtype A. An earlier study of sex workers in Senegal, published in 1999, found that women infected with subtype C, D or G were more likely to develop AIDS within five years of infection than those infected with subtype A.
Several studies conducted in Thailand suggest that people infected with CRF A/E progress faster to AIDS and death than those infected with subtype B, if they do not receive antiretroviral treatment.
Are there differences in transmission?
It has been observed that certain subtypes/CRFs are predominantly associated with specific modes of transmission. In particular, subtype B is spread mostly by homosexual contact and intravenous drug use (essentially via blood), while subtype C and CRF A/E tend to fuel heterosexual epidemics (via a mucosal route).
Whether there are biological causes for the observed differences in transmission routes remains the subject of debate. Some scientists, such as Dr Max Essex of Harvard, believe such causes do exist. Among their claims are that subtype C and CRF A/E are transmitted much more efficiently during heterosexual sex than subtype B.However, this theory has not been conclusively proven.
More recent studies have looked for variation between subtypes in rates of mother-to-child transmission. One of these found that such transmission is more common with subtype D than subtype A. Another reached the opposite conclusion (A worse than D), and also found that subtype C was more often transmitted that subtype D. A third study concluded that subtype C is more transmissible than either D or A. Other researchers have found no association between subtype and rates of mother-to-child transmission.
Is it possible to be infected more than once?
Until about 1994, it was generally thought that individuals do not become infected with multiple distinct HIV-1 strains. Since then, many cases of people coinfected with two or more strains have been documented.
All cases of confection were once assumed to be the result of people being exposed to the different strains more or less simultaneously, before their immune systems had had a chance to react. However, it is now thought that “superinfection” is also occurring. In these cases, the second infection occurred several months after the first. It would appear that the body’s immune response to the first virus is sometimes not enough to prevent infection with a second strain, especially with a virus belonging to a different subtype. It is not yet known how commonly super infection occurs, or whether it can take place only in special circumstances.
Do HIV antibody tests detect all types, groups and subtypes?
Initial tests for HIV are usually conducted using the EIA (or ELISA) antibody test or a rapid antibody test.
Compared with first generation EIA antibody tests that were initially developed, third and fourth generation EIA antibody tests are significantly more accurate. Unlike previous tests, the fourth generation test detects HIV antibodies and antigens simultaneously. The WHO recommends that tests should have an accuracy rate of 99 percent and whilst most do, this may vary slightly between the test brands.
The most-up-to date (fourth generation) EIA tests detect both HIV-1 and HIV-2 infections. Although most HIV infections are HIV-1 group M, EIA tests are also able to detect infections with rare groups and subtypes.
However, as HIV-2 and group O infections are extremely rare in most countries, routine screening programs might not be designed to test for them.Anyone who believes they may have contracted HIV-2, HIV-1 group O or one of the rarer subtypes of group M should seek expert advice.
What are the treatment implications?
An HIV positive man sitting at home before taking his antiretroviral drugs
Although most current HIV-1 antiretroviral drugs were designed for use against subtype B, there is no compelling evidence that they are any less effective against other subtypes. Nevertheless, some subtypes may be more likely to develop resistance to certain drugs, and the types of mutations associated with resistance may vary. This is an important subject for future research.
The effectiveness of HIV-1 treatment is monitored using viral load tests. It has been demonstrated that some viral load tests are sensitive only to subtype B and can produce a significant underestimate of viral load if used to process other strains. The latest tests do claim to produce accurate results for most Group M subtypes, though not necessarily for Group O. It is important that health workers and patients are aware of the subtype/CRF they are testing for and of the limitations of the test they are applying.
Not all of the drugs used to treat HIV-1 infection are as effective against HIV-2. In particular, HIV-2 has a natural resistance to NNRTI antiretroviral drugs and they are therefore not recommended. As yet there is no FDA-licensed viral load test for HIV-2 and those designed for HIV-1 are not reliable for monitoring the other type. Instead, response to treatment may be monitored by following CD4+ T-cell counts and indicators of immune system deterioration. More research and clinical experience is needed to determine the most effective treatment for HIV-2.
What are the implications for an AIDS vaccine?
The development of an AIDS vaccine is affected by the range of virus subtypes as well as by the wide variety of human populations who need protection and who differ, for example, in their genetic make-up and their routes of exposure to HIV. In particular, the occurrence of super infection indicates that an immune response triggered by a vaccine to prevent infection by one strain of HIV may not protect against all other strains. The increasing variety of sub-types found within countries suggests that the effectiveness of a vaccine is likely to vary between populations, unless an innovative method is developed which guards against many virus strains.
Inevitably, different types of candidate vaccines will have to be tested against various viral strains in multiple vaccine trials, conducted in both high-income and developing countries
OPPORTUNISTIC INFECTIONS
- WHAT ARE OPPORTUNISTIC INFECTIONS?
- TESTING FOR OIs
- OIs AND AIDS
- WHAT ARE THE MOST COMMON OIs?
- PREVENTING OIs
- TREATING OIs
WHAT ARE OPPORTUNISTIC INFECTIONS?
In our bodies, we carry many germs – bacteria, protozoa, fungi, and viruses. When our immune system is working, it controls these germs. But when the immune system is weakened by HIV disease or by some medications, these germs can get out of control and cause health problems.
Infections that take advantage of weakness in the immune defenses are called “opportunistic”. The phrase “opportunistic infection” is often shortened to “OI”.
TESTING FOR OIs
You can be infected with an OI, and “test positive” for it, even though you don’t have the disease. For example, almost everyone with HIV tests positive for Cytomegalovirus (CMV). But it is very rare for CMV disease to develop unless the CD4 cell count drops below 50, a sign of serious damage to the immune system.
To see if you’re infected with an OI, your blood might be tested for antigens (pieces of the germ that causes the OI) or for antibodies (proteins made by the immune system to fight the germs). If the antigens are found, it means you’re infected. If the antibodies are found, you’ve been exposed to the infection. You may have been immunized against the infection, or your immune system may have? cleared? the infection, or you may be infected. If you are infected with a germ that causes an OI, and if your CD4 cells are low enough to allow that OI to develop, your health care provider will look for signs of active disease. These are different for the different OIs.
OIs AND AIDS
People who aren’t HIV-infected can develop OIs if their immune systems are damaged. For example, many drugs used to treat cancer suppress the immune system. Some people who get cancer treatments can develop OIs.
HIV weakens the immune system so that opportunistic infections can develop. If you are HIV-infected and develop opportunistic infections, you might have AIDS.
In the US, the Center for Disease Control (CDC) is responsible for deciding who has AIDS. The CDC has developed a list of about 24 opportunistic infections. If you have HIV and one or more of these “official” OIs, then you have AIDS. The list is available at http://www.aidsmeds.com/lessons/StartHere8.htm.
WHAT ARE THE MOST COMMON OIs?
In the early years of the AIDS epidemic, OIs caused a lot of sickness and deaths. Once people started taking strong antiretroviral therapy (ART), however, a lot fewer people got OIs. It’s not clear how many people with HIV will get a specific OI.
In women, health problems in the vaginal area may be early signs of HIV. These can include pelvic inflammatory disease and bacterial vaginosis, among others. See fact sheet 610 for more information.
The most common OIs are listed here, along with the disease they usually cause, and the CD4 cell count when the disease becomes active:
- Candidiasis (Thrush) is a fungal infection of the mouth, throat, or vagina. CD4 cell range: can occur even with fairly high CD4 cells.
- Cytomegalovirus (CMV) is a viral infection that causes eye disease that can lead to blindness.CD4 cell range: under 50.
- Herpes simplex viruses can cause oral herpes (cold sores) or genital herpes. These are fairly common infections, but if you have HIV, the outbreaks can be much more frequent and more severe. They can occur at any CD4 cell count.
- Malaria is common in the developing world. It is more common and more severe in people with HIV infection.
- Mycobacterium avium complex (MAC or MAI) is a bacterial infection that can cause recurring fevers, general sick feelings, problems with digestion, and serious weight loss. CD4 cell range: under 75.
- Pneumocystis pneumonia (PCP) is a fungal infection that can cause a fatal pneumonia. CD4 cell range: under 200. Unfortunately this is still a fairly common OI in people who have not been tested or treated for HIV.
- Toxoplasmosis (Toxo) is a protozoal infection of the brain. T-cell range: under 100.
- Tuberculosis (TB) is a bacterial infection that attacks the lungs, and can cause meningitis. CD4 cell range: Everyone with HIV who tests positive for exposure to TB should be treated.
PREVENTING OIs
Most of the germs that cause OIs are quite common, and you may already be carrying several of these infections. You can reduce the risk of new infections by keeping clean and avoiding known sources of the germs that cause OIs.
Even if you’re infected with some OIs, you can take medications that will prevent the development of active disease. This is called prophylaxis. The best way to prevent OIs is to take strong ART. See Fact Sheet 403 for more information on ART.
The Fact Sheets for each OI have more information on avoiding infection or preventing the development of active disease.
TREATING OIs
For each OI, there are specific drugs, or combinations of drugs, that seem to work best. Refer to the Fact Sheets for each OI to learn more about how they are treated.
Strong antiretroviral drugs can allow a damaged immune system to recover and do a better job of fighting OIs. Fact Sheet 481 on Immune Restoration has more information on this topic
Complications
HIV infection weakens your immune system, making you highly susceptible to numerous infections and certain types of cancers.
Infections common to HIV/AIDS
- Tuberculosis (TB). In resource-poor nations, TB is the most common opportunistic infection associated with HIV and a leading cause of death among people with AIDS. Millions of people are currently infected with both HIV and tuberculosis, and many experts consider the two diseases to be twin epidemics.
- Salmonellosis. You contract this bacterial infection from contaminated food or water. Signs and symptoms include severe diarrhea, fever, chills, abdominal pain and, occasionally, vomiting. Although anyone exposed to salmonella bacteria can become sick, salmonellosis is far more common in HIV-positive people.
- Cytomegalovirus. This common herpes virus is transmitted in body fluids such as saliva, blood, urine, semen and breast milk. A healthy immune system inactivates the virus, and it remains dormant in your body. If your immune system weakens, the virus resurfaces — causing damage to your eyes, digestive tract, lungs or other organs.
- Candidiasis. Candidiasis is a common HIV-related infection. It causes inflammation and a thick, white coating on the mucous membranes of your mouth, tongue, esophagus or vagina. Children may have especially severe symptoms in the mouth or esophagus, which can make eating painful.
- Cryptococcal meningitis. Meningitis is an inflammation of the membranes and fluid surrounding your brain and spinal cord (meninges). Cryptococcal meningitis is a common central nervous system infection associated with HIV, caused by a fungus found in soil. The disease may also be associated with bird or bat droppings.
- Toxoplasmosis. This potentially deadly infection is caused by Toxoplasma gondii, a parasite spread primarily by cats. Infected cats pass the parasites in their stools, and the parasites may then spread to other animals and humans.
- Cryptosporidiosis. This infection is caused by an intestinal parasite that’s commonly found in animals. You contract cryptosporidiosis when you ingest contaminated food or water. The parasite grows in your intestines and bile ducts, leading to severe, chronic diarrhea in people with AIDS.
Cancers common to HIV/AIDS
- Kaposi’s sarcoma. A tumor of the blood vessel walls, this cancer is rare in people not infected with HIV, but common in HIV-positive people.
Kaposi’s sarcoma usually appears as pink, red or purple lesions on the skin and mouth. In people with darker skin, the lesions may look dark brown or black. Kaposi’s sarcoma can also affect the internal organs, including the digestive tract and lungs.
- Lymphomas. This type of cancer originates in your white blood cells and usually first appears in your lymph nodes. The most common early sign is painless swelling of the lymph nodes in your neck, armpit or groin.
Other complications
- Wasting syndrome. Aggressive treatment regimens have reduced the number of cases of wasting syndrome, but it still affects many people with AIDS. It’s defined as a loss of at least 10 percent of body weight, often accompanied by diarrhea, chronic weakness and fever.
- Neurological complications. Although AIDS doesn’t appear to infect the nerve cells, it can cause neurological symptoms such as confusion, forgetfulness, depression, anxiety and difficulty walking. One of the most common neurological complications is AIDS dementia complex, which leads to behavioral changes and diminished mental functioning.
- Kidney disease. HIV-associated nephropathy (HIVAN) is an inflammation of the tiny filters in your kidneys that remove excess fluid and wastes from your bloodstream and pass them to your urine. Because of a genetic predisposition, the risk of developing HIVAN is much higher in blacks.
Regardless of CD4 count, antiretroviral therapy should be started in those diagnosed with HIVAN.
AIDS Stakeholders – Institutions Involved in HIV/AIDS Response in Moldova
At the national level, the state policy in the area of HIV/AIDS is implemented through the National Programme on Prevention and Control of HIV/AIDS and STI, which determines national strategies of priority for prevention, epidemiological surveillance and treatment. The structure of the institutional framework of the NAP is rather complex. The main executors of the state policy in the area of HIV/AIDS and STI are the Government, local public administration authorities, Ministry of Health and Social Protection and other Ministries, NGOs, mass media, etc. An important contribution is carried out by international organizations, such as UNAIDS and most UN agencies, GFATM/WB, Soros Foundation Moldova, SIDA, etc.
National AIDS Stakeholders and their Role
National Coordination Council and NCC Secretariat
- Development, integration, correlation and monitoring of activities under the NAP
Government and its Ministries
- Capacity building related to national response to HIV/AIDS/STI;
- Support to the consolidation of NGO networks which are working in the field of HIV/AIDS/STI and people living with HIV/AIDS;
- Priority financing, political support of HIV/AIDS activities;
- Focal points and HIV related responsibilities under several ministries;
- M&E
Local Public Administration Authorities
- Regional interdepartmental, multisectoral HIV/AIDS/STIs committees;
- Earmarking in local budgets for HIV/AIDS activities;
- Contribution to regional programmes in the field.
Mass Media
- Promote and make use of non-discriminatory language in HIV/AIDS/STIs
- Communication activities.
National Centre for Public Health
- Evaluation of population health, prognosis as to the evolution of basic indicators and sanitary-epidemiological statistics;
- Elaboration of prevention programmes at national and territorial levels;
- Fighting negative effect of harmful environment and production factors;
- Cooperation with other medical-sanitary national and international institutions of common and global interest;
- Exchange of experience and information.
Public Institution “UCIMP”
- Strengthening of the public health through reforming the health system;
- Development of the institutional capacities;
- Fighting negative effect of harmful environment and production factors;
- Support to the National Programmes on Prevention and Control of HIV/AIDS/STI and TB and National Programmeon Blood Transfusion Safety.
Rayon Centres for Preventive Medicine
- Epidemiological surveillance in territories;
- Elaboration and implementation of preventive measures;
- Organization and coordination activities with other medical institutions.
National AIDS Centre
- Analysis of the epidemiological situation, maintenance of official statistics;
- Elaboration of methods in all the areas of activity;
- Confirmation and reference tests for HIV/AIDS;
- Training and seminars on HIV/AIDS for family doctors.
Republican Dermato-Venerological Dispensary
- ARV treatment;
- Treatment of opportunistic infections.
National Centre for Health Management
- Health system strengthening;
- Scientific research coordination in the field of public health;
- Development of the legislative framework in public health.
Monitoring and Evaluation Unit on HIV/AIDS
- Development of M&E plans for the National AIDS Programmes, UNGASS reports, etc.
NGOs
- Grassroots activities;
- Wide range of prevention, care, support and rehabilitation projects in HIV/AIDS related areas;
Lobby and advocacy.
International organizations
Financial and technical assistance.
Association “Positive initiative”
“Positive initiative” is a new created association that represents a network within the organizations with a reach experience in the field of HIV, especially working and providing services for MARPS (Most at Risk populations), people living with HIV, IDU, women and children HIV+ or affected by HIV.
Association “Youth for Right to Life”, Balti
Association “Youth for Right to Life”, Balti is an NGO from Balti, Republic of Moldova, that more than one decade works in the field of HIV prevention, drug abuse and social assistance.
UN Groups on HIV/AIDS
Coordination, cohesion and effectiveness of the UN contribution to the national response to HIV/AIDS
More information on UN TG and UN JT
UNAIDS
Advocacy, Capacity building (NCC, TWG, NGOs, PLH, etc), Promotion of best practices, Support of PLH
WHO
Advocacy, ARV Treatment, Technical norms and guidelines, Promotion of research into health service delivery
UNICEF
Advocacy, Children made vulnerable or orphaned because of HIV, Prevention of Mother to Child Transmission, Life skills based education, Prevention among young people
UNFPA
Advocacy, Reproductive Health, Condom Promotion, Peer education, VCT
UNDP
Advocacy, Coordination, HIV Prevention in the Armed Forces
IOM
HIV and Migrants
UNHCR
HIV and Refugees
ILO
HIV at the workplace
UNESCO
HIV Prevention education
WFP
Nutrition and food security for PLHIV and their families
UNODC
HIV prevention among IDU and in penitentiaries
WB
Advocacy, Financial support
UNIFEM
Prevention of HIV among women
Other Stakeholders
AFEW – AIDS Foundation East West
Campaign on Stigma and Discrimination against PLH, HIV Prevention Campaign
Soros Foundation – Moldova
Harm Reduction, Palliative Care
Center for Health Policies and Studies
Contribute to health system development, support reforms and capacity building in HIV/AIDS and TB area
SIDA – Swedish International Development Agency
Strengthening Civil Society, Prevention of Social Exclusion and Promotion of Public Health
MSF – MédecinsSansFrontières
Setting up operations in Moldova that will address the needs of both TB and HIV patients
USAID Moldova
Prevention of HIV/AIDS and Viral Hepatitis B&C
Positive Initiative
A network within the organizations with a reach experience in the field of HIV
Youth-friendly Health Centre “ATIS”
Youth friendly services, IEC activities
UOHR – Union of Harm Reduction Organizations
Coordinating, building capacity, and providing support to organizations operating in the field of harm reduction
League of People Living with HIV of Republic of Moldova
Advocacy and support for people living with HIV
Moldova AIDS Network
Transfer of experience and capacity building in the field of HIV/AIDS, STI and Drug-abuse prevention
Non-governmental Organization “New Life”
Promote the healthy life style and rehabilitation
Foster ecumenical cooperation, increase the role of the Churches in Moldavian modern society
MIHR – Moldova Institute for Human Rights
Education, promotion and defense of rights and freedoms foreseen by the national and international legislation
NYRC – National Youth Resource Centre
Network to promote services targeting young people
Charity Social-Medical Foundation “Angelus Moldova”
Palliative care and psychological support
CRS – Catholic Relief Services
Hope, security and opportunity
GTZ – German Technical Cooperation Bureau
Sustainable development, improvement of people’s living conditions
Advocacy, campaigning activities and lobby
Association “TineretulPozitiv”
Protection of rights of young people affected by HIV/AIDS
Information Center “GenderDoc-M”
Lobby and protection of rights of LGBT community representatives
Moldova Youth Peer Education Network
Promotion of peer to peer education
Association “Youth for the right to live”
HIV Prevention, drug abuse and social assistance
